At the end of my first year at UVM in 2023, I found myself sitting on my much too uncomfortable and insatiably loud plastic mattress with tears rolling down my face.
The housing accommodations my doctor and I requested to aid in my continued recovery from an eating disorder were denied without reason.
This denial letter entered my inbox during the Week of Body Positivity and Eating Disorder Programming, hosted by the Center for Health and Wellbeing. These contradicting actions from Residential Life and Student Accessibility Services left me confused.
While confusing, it sparked my interest in understanding how UVM handles concerns related to eating disorders on campus.
UVM offers the Catamount Recovery Program, where students who struggle with substance use can get priority registration, access to therapeutic recovery groups, collaborations with student health services and on-campus recovery housing.
However, for eating disorders, the University website only directs students to Student Health Services to meet with a physician and promotes Body Positivity Week, as mentioned above.
According to the National Eating Disorders Association, the highest-risk age group for developing eating disorders is 18 to 21. They also estimate that 10-20% of women and 4-10% of men in college suffer from an eating disorder.
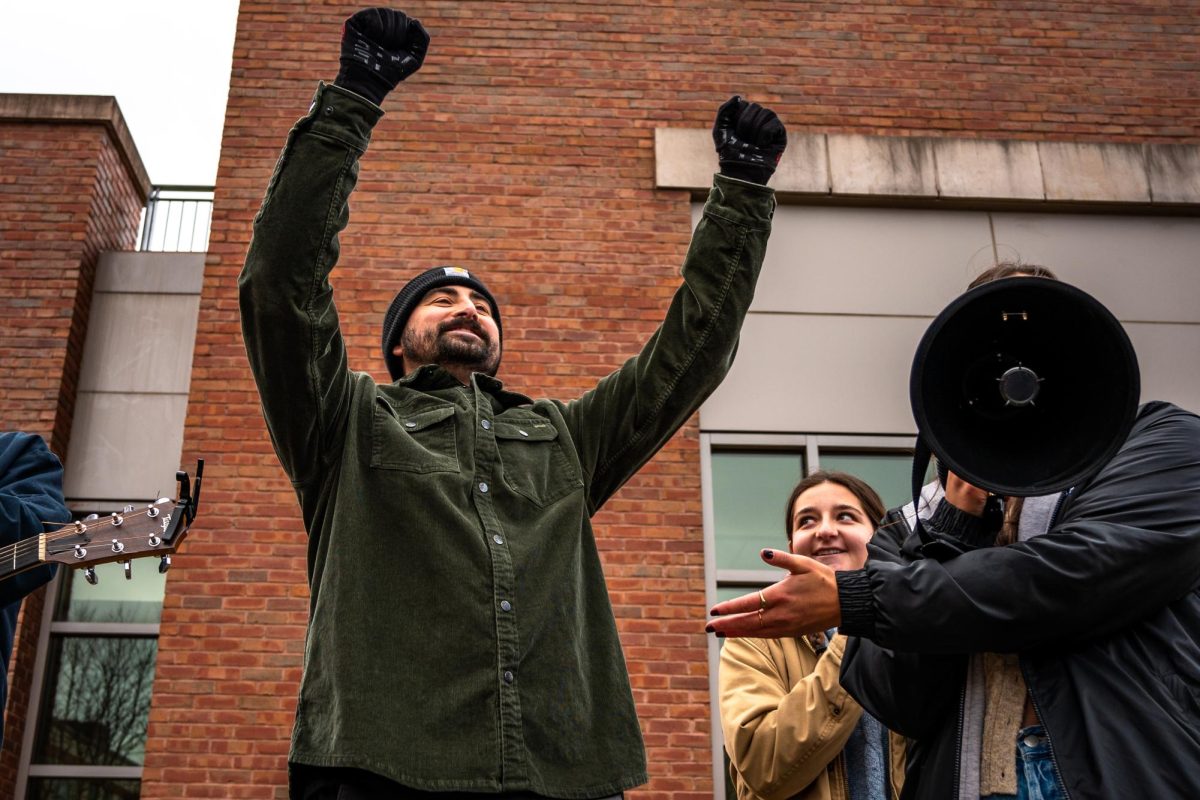
Sophomore Lauren Knopp, who is in recovery from an eating disorder, highlights the recent layoffs of eight Living Well staff as a focal point to why she no longer feels supported on campus.
“It’s been difficult certainly, because now that’s not somewhere I feel very comfortable going to knowing that it’s understaffed, it’s not as frequently open,” said Knopp.
Knopp has been in recovery for four years, and when asked if she would feel supported on campus in the case of a relapse, she lacked confidence.
“I don’t think so at the moment. It’s a sad reality, but also I think the severity of what an eating disorder is is very understated,” said Knopp.
Licensed psychiatrist Anne Clegg and registered dietician Amy Sercel who both work for UVM’s Center for Health and Wellbeing helped me understand the gap in campus resources.
Although there seemed to be minimal resources on campus, I learned that might not be entirely true.
CHWB counselors, dieticians, nurse practitioners and psychiatrists have formed a focus group to support students.
“[It’s] an interdisciplinary team where [they] connect and collaborate to support students who are in recovery or struggling with an eating disorder,” said Sercel.
While Sercel is the only dietician at Student Health Services, she noted there are two additional dieticians working under UVM Dining. However, on their website, there is only one registered dietician listed, Ania Egan.
Sercel also co-facilitates a body-positive group with Counseling and Psychiatry Services therapist Kelly Boardman.
“The aim of that group is to help students examine the messages they’ve gotten about health, weight, eating disorders and recovery,” said Sercel.
The group is open to all students, but she said that it is predominantly attended by those in recovery from an eating disorder.
Clegg touched on the loss of Living Well staff, specifically Annie Valentine, an education and training manager, and how that has impacted CHWB’s ability to reach students in need.
“Annie was really a champion for students, and shared very openly about her own struggles, and was just a really important contact for people,” said Clegg.
There are also many resources for student-athletes on campus, specifically a program focused on RED-S, or relative energy deficiency in sports. The syndrome develops from a lack of sufficient fuel through food to supply energy for the athletic performance needs of the athlete, according to the Boston Children’s Hospital.
Sercel partners with the sports medicine team and two sports psychologists in order to support athletes that are unable to adequately meet their nutrition needs.
She also holds a supportive lunch group in collaboration with athletic counselor, Mollie Gribbin, that is held in the Living Well studio each month.
While these resources are beneficial, they are still somewhat limited. Each student has access to counselors at CAPS but are limited to six sessions with them per semester, Clegg said. For students experiencing acute mental health issues, this may not be sufficient.
Clegg noted the University’s inability to help students at all levels of care.
“We can’t be everything for everybody, as much as we want to help people in a system, often the system does require that students might have to step out of what UVM can offer,” she said.
The Kahm Clinic in Winooski is an important community resource to Clegg, for a higher level of care than UVM offers. They offer in-person intensive outpatient programming as well as partial-hospitalization programming.
There is clearly a need for increased advertising of mental health services offered by UVM. While there are programs and people willing to help, they aren’t beneficial if no one knows about them.
If the campus does not offer what you need, there is someone in CHWB who can help direct you to an off-campus professional who will fit your needs.
Through reaching out about resources on campus, I feel more confident in UVM’s ability to support people with eating disorders. However, there is definitely room for improvement in terms of housing accommodation, accessibility, outreach and the formation of a stronger recovery community on campus.
For an increased sense of safety, the word must be spread about the programs and resources available to students who are struggling with eating disorders to ensure that no one feels alone.