Editor’s note: Ciara Lordan is a second year nursing student at UVM and a student in CNHS’s Research in Nursing course.
The healthcare field is often revered for its innovative research efforts and dedication to bettering the lives of the people it serves.
Traditionally, physicians, medical scientists and other research-focused professionals have received the majority of this attention. What many may not know is the essential role that nurses perform in research settings, whether it be through their own research or as part of a larger research team.
“Nurses bring a really important perspective because we are the providers that are with patients really 24/7/365,” said Dr. Cynthia Peterson, assistant nurse manager and nurse scientist at UVM Medical Center.
Through her role at UVMMC, Peterson is able to both support the development of new evidence-based practice initiatives as well as work on her own projects, having led resilience workshops as part of the Changing Minds, Changing Lives project since 2021.
Peterson’s research primarily investigates improvements for nurses in the workplace, including topics such as resilience in nursing, coping with stress in the profession and inclusion and belonging in healthcare teams.
Now more than ever, visibility for nursing research is growing. At UVMMC specifically, programs are being developed to allow nurses more designated time to work on research projects, said Peterson.
Even with this new attention and appreciation given to the advancement of nursing research at UVMMC, there are still barriers to getting research projects off the ground.
Melinda Pariser-Schmidt, clinical nurse project manager at UVMMC with a masters in nursing leadership, experienced these barriers firsthand when she developed her own quality improvement project in UVMMC’s neonatal intensive care unit.
UVMMC’s NICU has taken an innovative approach to their treatment of neonatal abstinence syndrome, a condition in which infants experience withdrawal due to exposure to substances such as opioids in utero.
Their previous approach relied on outpatient clinics to wean affected infants off of pharmacological interventions such as methadone. After initial hospital stays, infants were sent home on a steady dose of these medications to address their withdrawal symptoms and attend regular outpatient appointments.
However, in the wake of the COVID-19 pandemic, clinics were no longer able to support this approach and infants had to receive their treatment in the NICU, which lengthened their stay and overwhelmed nurses’ workloads, said Pariser-Schmidt.
It was at this time that Pariser-Schmidt was made aware of a new responsive bassinet that could ease the burden on nurses. The bassinet was able to respond to the infant’s needs for soothing and comfort by rocking and playing white noise while simultaneously observing safe sleep protocols.
Pariser-Schmidt contacted the manufacturer of the bassinets and initiated a quality improvement project using the bassinets for infants affected by neonatal abstinence syndrome.

“We’d never done anything like this before,” she said. “We’d never had a nursing-led quality improvement project of this sort of scope and scale.”
It took about a year for Pariser-Schmidt to get her project running. As a nurse pursuing a research project, Pariser-Schmidt faced many obstacles and “red tape” in a research system designed for physicians and other medical researchers, not nurses.
Pariser-Schmidt noted that she was unable to submit her own application for her project to be approved by an institutional review board, the group tasked with ensuring all research involving human subjects adheres to established regulations.
Instead, she had a physician colleague who had access to the portal submit it for her. She was also unable to access the same grant management systems that physicians have access to, Pariser-Schmidt said.
Despite the roadblocks, Pariser-Schmidt successfully conducted her quality improvement project, finding that the responsive bassinets decreased the length of stay by 17% and increased the quality of sleep by 42% in infants with fetal abstinence syndrome.
Because of these findings, the bassinets are now common practice in UVMMC’s NICU, she said.
This project earned Pariser-Schmidt UVMMC’s Vision Award in 2022, an honor that has historically been granted to mostly physicians, she said.
“Anytime you’re doing anything as a nurse from a nursing lens, you are inherently taking a different view of both the problem and the potential solution,” she said. “As a nurse, you are trained at your very baseline to be an advocate.”
In addition to UVMMC’s dedication to furthering nursing research, UVM’s College of Nursing and Health Sciences is also working to expand its nursing research programs.
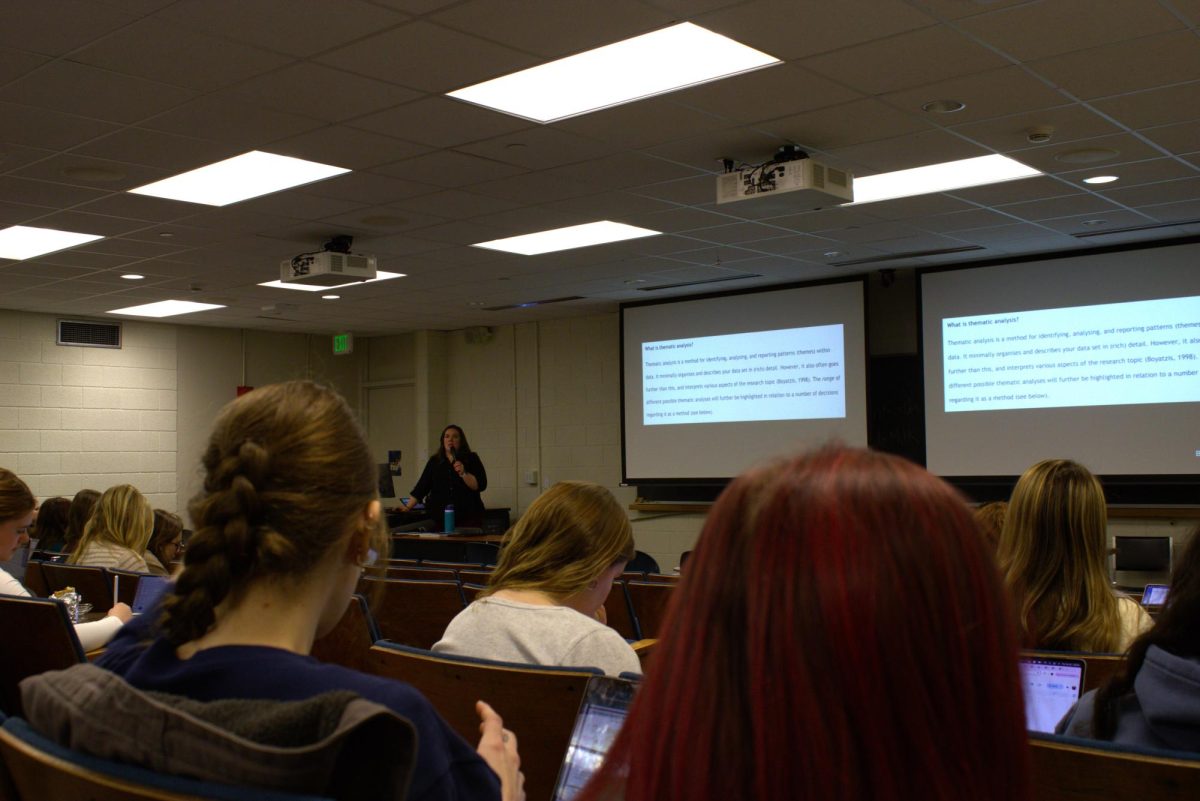
UVM’s undergraduate nursing program incorporates a Research in Nursing course, which was recently restructured by nursing professor Dr. Laura Lewis into its standard curriculum for all BSN candidates.
The course aims to expose nursing students to the field of nursing research and its opportunities in an active manner, rather than a traditional lecture-style course, said Dr. Kathleen Monforte, current instructor of Research in Nursing and clinical assistant professor in the department of nursing.
Monforte is a nurse researcher who studies effective learning environments for nursing education. She became interested in nursing research after taking a similar course while in nursing school, in addition to seeing quality improvement projects while working in a clinical setting, she said.
Nursing research combines the critical thinking of scientific disciplines with compassion and care, taking a preventative approach to problem-solving, said Monforte.
“The nursing perspective is different because it’s the science and art put together,” she said. “We add in a level of compassion and empathy.”
Due to her research efforts, Monforte has been able to apply her findings to her work, modeling her course instruction after what she has found to be the most effective teaching strategies for nursing education, she said.
Similarly, senior nursing student Gabrielle Railey, undergraduate teaching assistant for the Research in Nursing course, also found a passion for research through the class, she said.
“I felt kind of stuck in nursing but this [course] just opened my mind and now I’m very interested in becoming a nurse researcher and participating in research after I graduate,” Railey said.
Railey, who has been a TA for the course for two years, was interested in learning more about nursing opportunities beyond traditional bedside nursing roles, and through the course was able to see how nurses can be impactful in other settings, including in research, she said.
CNHS faculty are not only supporting the field of nursing research within the classroom, but they are also furthering the field with their own research.
Currently, there is a diverse array of research being completed by clinical faculty from CNHS, said Dr. Paula Deming, associate dean for faculty affairs and research in CNHS.
“In the last five years, there’s been an emphasis on the importance of nurses and in particular, nursing research, in helping to inform patient care and better patient outcomes,” Deming said. “Nursing research informs clinical practice and can actually help to move forward change within healthcare systems.”
UVM has recognized this recent emphasis on nursing research and is aiming to support and aid the research endeavors within the nursing department. Deming’s position within the college specifically helps to facilitate research through mentorship, organization of grants and support for proposals, she said.
CNHS’s research program in particular has an advantage due to its proximity to UVMMC. This connection between the college and a major hospital allows for research to be applied to a clinical setting, which has been monumental for the advancement of research projects, said Deming.
While nursing research has seen an increase in popularity and visibility in recent years, Peterson predicts that the field will continue to grow.
“Having nursing guide quality improvement and research from the bedside is critical to not only the evolution of nursing but the sustainability of healthcare overall,” said Pariser-Schmidt.