People struggling with mental illness may feel hopeless, an experience often reinforced by the systems designed to help them.
If you pay attention to mental health advocacy in the media, you may have noticed a recurring message: if you’re struggling, reach out. Resources are always available.
Constant assurance in schools, workplaces and on social media that people struggling with mental illness can resort to group therapy, counseling, psychiatry and more gives the impression that the issue can easily be resolved.
As a psychology major, I can say with confidence that these methods are great. Although these resources are not necessarily permanent solutions, they can definitely serve as effective treatment, making life easier for those who are able to access them. Unfortunately, many people who struggle cannot.
If you lack experience in the domain of mental health treatment in today’s world, you may assume that most people have access to resources. I sure did before I actually began looking into treatment for myself.
I began struggling with my mental health in middle school. Although I often felt debilitated by my struggles, I survived without treatment for years, and only began to look for support during my sophomore year of high school.
My close friends have been my biggest resource. It is important to know that you are not burdening others by relying on them for support, but also recognize that friends are not equipped to serve as a replacement for therapy.
I received help from my high school guidance counselor, too, but my unwillingness to communicate my challenges with my very distant parents left me unable to access professional resources prior to college.
I was hopeful that upon arriving at the UVM, I would easily be able to utilize Counseling and Psychiatry Services or be referred to providers in the area without having to involve my parents in the process.
However, not only was it difficult to schedule counseling appointments, but I was met with the harsh reality that my insurance as an out-of-state student would not cover my psychiatry through CAPS. In fact, my insurance would cover virtually nothing in the entire state of Vermont.
Upon realizing that counseling at UVM might be my only option, I felt extremely disheartened. The short-term model of five sessions per semester did not feel like sufficient care for the mental health crisis I’ve hardly been surviving through for the past six years.
So in the last few months, I have recognized that obtaining mental health treatment can not only be difficult for low-income families or others without good health insurance coverage, but for everyone.
As I’ve observed from my personal experiences, an obvious barrier when reaching out for mental health care is the crippling issue of insurance.
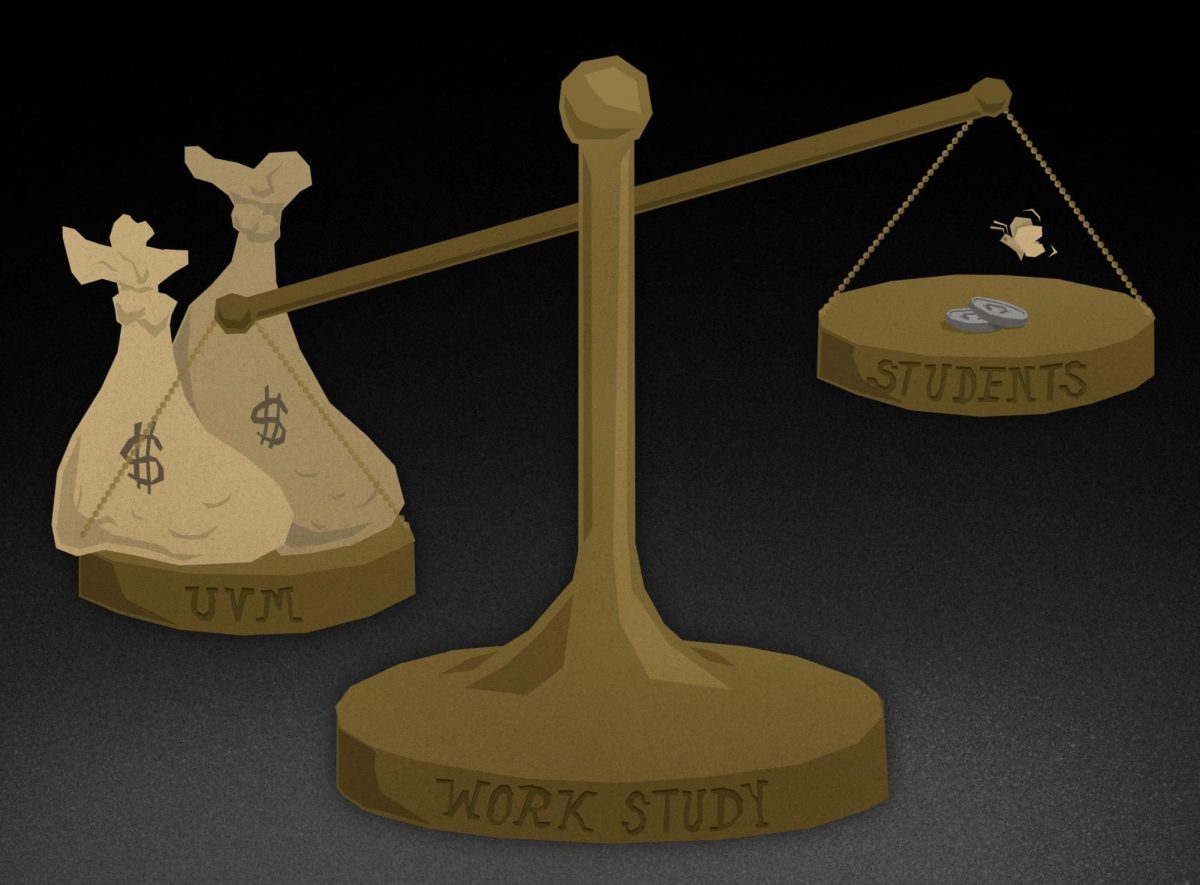
As of 2023, 10.9% of working Americans do not have health insurance, according to the National Center for Health Statistics. This amounts to around 37 million people.
With climbs of mental health treatment costs, research shows that patients with severe depression spend an average of $10,836 annually on healthcare costs, according to a May 10, 2021 CNBC article.
Even if you do have a somewhat decent health insurance plan and receive at least some counseling coverage, over half of all therapists don’t accept insurance, according to a June 14, 2023 Psychology Today article. The costs can be crippling without insurance coverage.
Or, if you’re like me and you’re an out-of-state student, there’s a good chance that you’re out-of-network and your health insurance is irrelevant anyways.
You could always resort to UVM’s Ship Health Insurance Plan, which is $4,478 annually. This does cover most counseling and psychiatry needs, but compounded with college tuition, it still may be inaccessible for many families.
There are still more challenges to face. For one, I greatly underestimated the endless wait.
Especially since the COVID-19 pandemic began, more people have been prioritizing their mental health, and so the demand for licensed mental health professionals has increased exponentially, according to the American Counseling Association. In the U.S., many individuals and families are unable to receive much needed help from licensed professionals.
Every practice seems to be booked solid. Even UVM Counseling and Psychiatry Services has a months-long waiting list.
Furthermore, it’s difficult to work mental health care into a college student’s schedule with so many other commitments already. Being met with limited hours—CAPS only being open weekdays 8:00 a.m. to 4:30 p.m.—can make things even more challenging.
I have had extremely productive and helpful counseling sessions, but the therapist I was set up with, one of the only available therapists at CAPS, only comes in three days a week, and so I have to jump through hoops to meet with her.
If you have anxiety, you’ll have to overcome that to even begin to take steps towards treating it.
A perfectly healthy person could hardly endure the exhaustion of trying to obtain mental health treatment. When you’re struggling with mental illness, the process is even more challenging.
The duality of society’s outlook on mental health treatment is beyond ironic, misleading and discouraging: it’s enough to make someone mentally ill.